"For most of my adult life, I've felt helpless about being overweight. When I met with a doctor a few years ago to discuss my high cholesterol, he held up a hunk of faux flesh meant to model a pound of excess fat and encouraged me to lose 20 of said gelatinous blobs. Perhaps, he suggested, I should eat less red meat and start exercising."
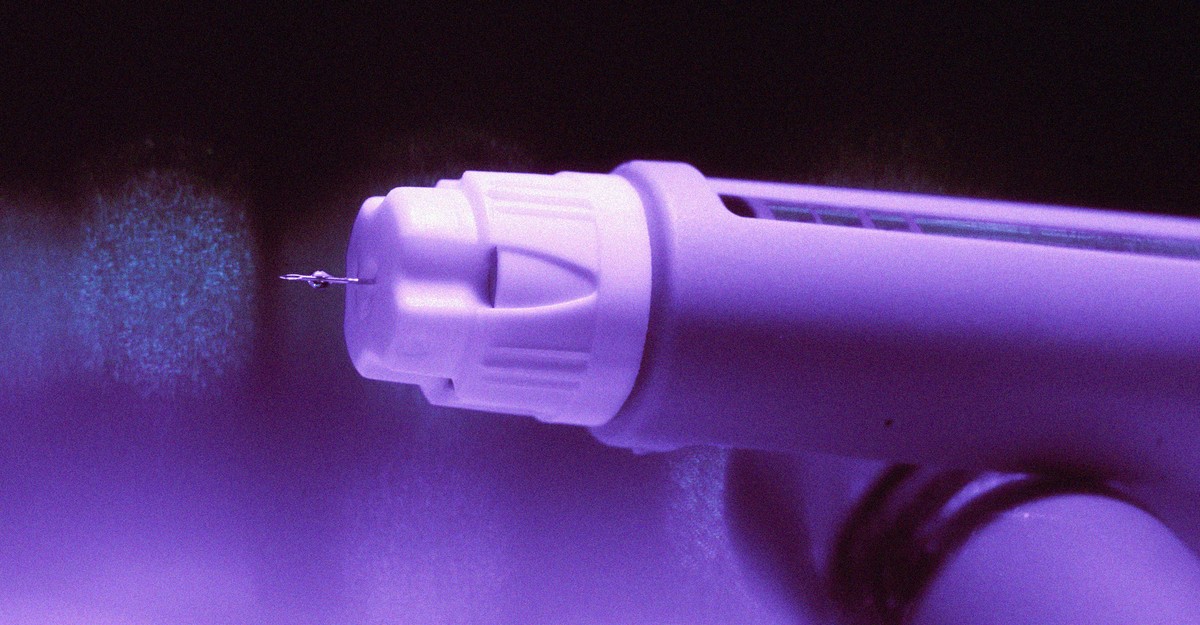
"Starting an obesity drug was supposed to be triumphant. The days of being winded after walking up the stairs to my apartment, and buying T-shirts marketed for guys with big bellies, would finally be over. Or so I thought. My health insurance didn't cover Wegovy or Zepbound, the two GLP-1 drugs approved for weight loss. (Both medications are also sold for diabetes, under the brand names Ozempic and Mounjaro, respectively.) Despite my pleading, the insurance company wouldn't budge."
A person experienced longstanding frustration with obesity and recounted a doctor who displayed a model pound of fat and urged substantial weight loss despite the person's regular gym routine and long-term vegetarianism. Beginning a GLP-1 obesity medication was expected to resolve mobility and clothing concerns, but private health insurance refused to cover Wegovy or Zepbound. Medicare is legally barred from covering these drugs for obesity. Initial manufacturing shortages constrained access, and although supply later improved, insurers increasingly deny coverage or impose barriers. GoodRx data show large shares of plans do not cover Zepbound and require prior steps for Wegovy.
Read at The Atlantic
Unable to calculate read time
Collection
[
|
...
]